CAKUT: Primer for Doctors
By Dr Poongkodi Nagappan
16th April 2025


Photo by Laura Garcia on Pexels
Functions of the Urinary Tract
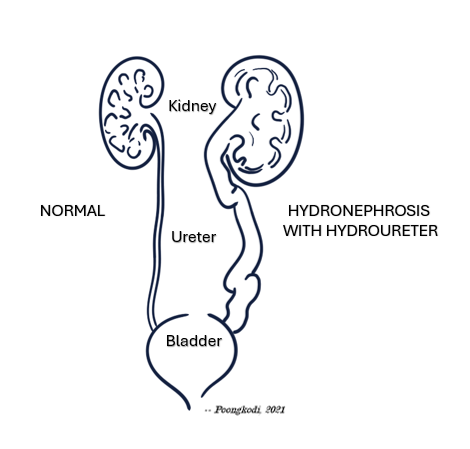
The kidney is connected to the urinary bladder by the ureter, and these organs function together as a single unit to remove waste products from the blood in the form of urine. The urinary tract transports, stores, and removes urine from the body. By doing so, it maintains the body's fluid, electrolyte, and acid-base balance. The kidneys also release hormones to control blood pressure, red blood cell production, and maintain bone health.
What is CAKUT?
CAKUT stands for Congenital Anomalies of the Kidneys and Urinary Tract. The term was first described in 1998 and was adopted into medical literature [1].
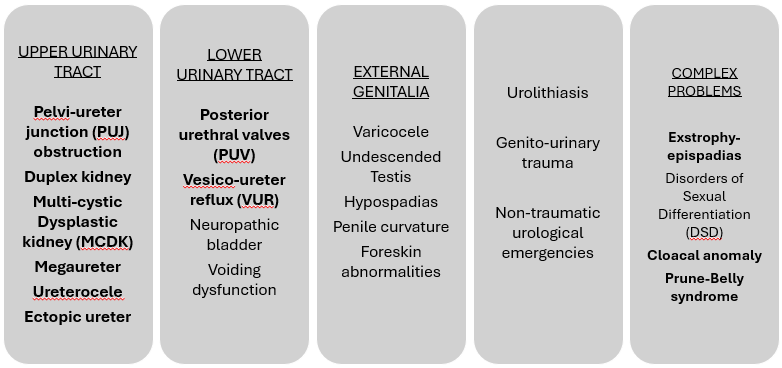
A wide range of structural anomalies of the urinary tract is included as part of CAKUT. Some common examples are multicystic dysplastic kidney, pelvi-ureteric junction obstruction, megaureter, duplication of the ureter, vesico-ureteric reflux, and posterior urethral valves.
The term CAKUT was introduced at a time when doctors believed that a single genetic mechanism caused all the malformations [2]. For day-to-day paediatric urology practice, a precise anatomical diagnosis is more helpful in patient management. The spectrum of paediatric urology conditions is shown below, with CAKUT conditions highlighted in bold.
How is CAKUT diagnosed?
CAKUT is most often diagnosed by prenatal foetal ultrasound. This is often performed in the second trimester of pregnancy to visualise the fetal kidneys, bladder, and amniotic fluid volume. It can also be detected on postnatal ultrasound performed for prolonged jaundice, urinary tract infection, failure to thrive, or as a screening test.
What causes CAKUT?
CAKUT is caused by a combination of genetic, maternal, and environmental factors. Only 12-20% of patients with CAKUT have mutations in single genes [3].
It may be an isolated condition or syndromic, which means CAKUT is part of other anomalies involving multiple organ systems. Down's syndrome is associated with a high prevalence of CAKUT, leading to chronic kidney disease in adulthood [4]. It is good clinical practice to perform an ultrasound of the urinary tract in children with Down's Syndrome.
Parents are mainly concerned about the risk of future siblings in the family developing CAKUT
Does my family need genetic counseling if we have a child with CAKUT?
Genetic counselling is an essential part of care, providing education and emotional support to parents. It may not be possible to determine the exact risk of inheritance of a disease because CAKUT is caused by a range of mechanisms. Genetic mutations may involve a single gene, multiple genes, or segments of chromosomes. There may be variations in gene expression. CAKUT can also develop as a result of foetal exposure during pregnancy [5].
Genetic testing is not widespread in Kuala Lumpur and the rest of Malaysia. However, it is still advisable to discuss genetic testing in patients with [5]
• Syndromic CAKUT
• Familial CAKUT, whereby other family members also have CAKUT, and there is consanguinity
• Sporadic CAKUT with a severe form of renal dysplasia
What is the incidence of CAKUT?
The incidence of CAKUT in Malaysia is not known. Studies done across the world estimate the prevalence of CAKUT to be between 4 per 10,000 to over 100 per 10,000 individuals [6]. Factors associated with increased risk of CAKUT are maternal factors such as older age, diabetes, and obesity, as well as premature and low-birth-weight infants.
What are the complications of CAKUT?
CAKUT encompasses a wide range of conditions of varying severity. The severe form of CAKUT can result in impaired urinary drainage leading to urinary tract obstruction, urinary tract infection, formation of urinary tract stones, high blood pressure, growth and developmental delay, and chronic kidney disease [7]. Unfortunately, chronic kidney disease begins and progresses silently, causing no obvious symptoms until there is significant loss of renal function.
How can I prevent CAKUT?
CAKUT is caused by a combination of inherited and environmental factors. Women who intend to get pregnant should avoid medications that could impact foetal kidney development. These medications include
• Angiotensin-converting enzyme (ACE) inhibitors and Angiotensin-receptor blockers (ARB), both medications used to treat hypertension
• Non-steroidal anti-inflammatory drugs (NSAIDS)
• Glucocorticoids
• Anti-epileptic medication
• Aminoglycoside antibiotics
Offspring born to mothers with diabetes and obesity are at increased risk of having CAKUT [8]. This needs to be looked into during antenatal care.
Key Takeaways for the Health Care Professional
Nephrogenesis occurs during the foetal period and is impacted by maternal health and preterm birth. The kidneys continue to grow and mature after birth, especially during the first few years of life. Environmental stressors during this period can impair renal function.
The obstetrician and neonatologist play a crucial role in minimising placental insufficiency, perinatal hypoxia, and infections. The paediatricians, paediatric nephrologists, and paediatric urologists are well-positioned to optimise the kidney health of the child with CAKUT during the period of greatest growth and maturation by ensuring correct nutrition and prevention of infections. As the child reaches adulthood, the physicians, nephrologists, and urologists play a role in managing the declining kidney reserve caused by comorbidity and aging [9].
Considering the medical landscape in Malaysia, it is my opinion that children with known risk factors for developing CAKUT would benefit from ultrasound studies.
Poongkodi Nagappan
16th April 2025
REFERENCES AND FURTHER READING
Yerkes E, Nishimura H, Miyazaki Y, Tsuchida S, Brock JW 3rd, Ichikawa I. Role of angiotensin in the congenital anomalies of the kidney and urinary tract in the mouse and the human. Kidney Int Suppl. 1998;67:S75-7. doi: 10.1046/j.1523-1755.1998.06715.x
Woolf AS. The term CAKUT has outlived its usefulness: the case for the prosecution. Pediatr Nephrol. 2022;37(11):2785-2791. doi: 10.1007/s00467-022-05576-4
Kolvenbach CM, Shril S, Hildebrandt F. The genetics and pathogenesis of CAKUT. Nat Rev Nephrol. 2023;19(11):709-720. doi: 10.1038/s41581-023-00742-9
Nine Knoers. When to perform genetic testing in CAKUT? ERKNet/ESPN Educational Webinars on Pediatric Nephrology & Rare Kidney Diseases 2022
Leskur M, Leskur D, Marijan S, Minarik L, Lozić B. Congenital Anomalies of the Kidney and Urinary Tract in Down Syndrome: prevalence, phenotypes, genetics and clinical management. Genes (Basel). 2025;16(3):245. doi: 10.3390/genes16030245
Hays T, Thompson MV, Bateman DA, et al. The prevalence and clinical significance of congenital anomalies of the kidney and urinary tract in preterm infants. JAMA Netw Open. 2022;5(9):e2231626. doi:10.1001/jamanetworkopen.2022.31626
Sanderson KR, Warady BA. End-stage kidney disease in infancy: an educational review. Pediatr Nephrol. 2020;35(2):229-240. doi: 10.1007/s00467-018-4151-8
Parimi M, Nitsch D. A systematic review and meta-analysis of diabetes during pregnancy and congenital genitourinary abnormalities. Kidney Int Rep. 2020;5(5):678-693. doi: 10.1016/j.ekir.2020.02.1027.
Chevalier RL. CAKUT: a pediatric and evolutionary perspective on the leading cause of CKD in childhood. Pediatr Rep. 2023;15:143-153. doi:10.3390/pediatric15010012
Description of urological conditions seen in my practice, diagnosis, and treatment
Collection of images and videos on my operations, preoperative preparation, and patient information
Find out more about health promotion and disease prevention
Study of history teaches us not to take ourselves too seriously
On-the-job training and navigating work-life beyond medical school
Find Out More
DISCLAIMERS
We advise you to consult a qualified urologist if you seek medical advice, diagnosis, or treatment
We are not liable for risks or issues associated with using or acting upon the information from this website
For doctors, the information provided on this website is for educational purposes only and it aims to support and not replace accredited urology training
For patients, we aim to provide sensible health care information that will support but not replace any in-depth discussion you may have with your own urologist